Solving the Scale-Up Barrier: How We Engineered a High-Yield, In Vivo-Ready T-Cell Process
Context and Challenge
It often surprises cell therapy developers that their lab-scale process doesn’t perform well at larger scale. It uses excessive resources, depends on manual steps, carries contamination risks and delivers unpredictable outcomes. Without a process optimized from the start, you end up spending more time troubleshooting than moving your program forward.
To demonstrate how a proactive approach pays off, we undertook an internal project. Following a successful T-flask proof-of-concept, we focused on optimizing the T-cell process and making it scalable. This new process was then successfully rolled out for in vivo studies. We wanted to share the practical approach we used to achieve that efficiency and de-risk the development path.
Our Approach
1. Cutting Cost and Labor in T‑Cell Culture
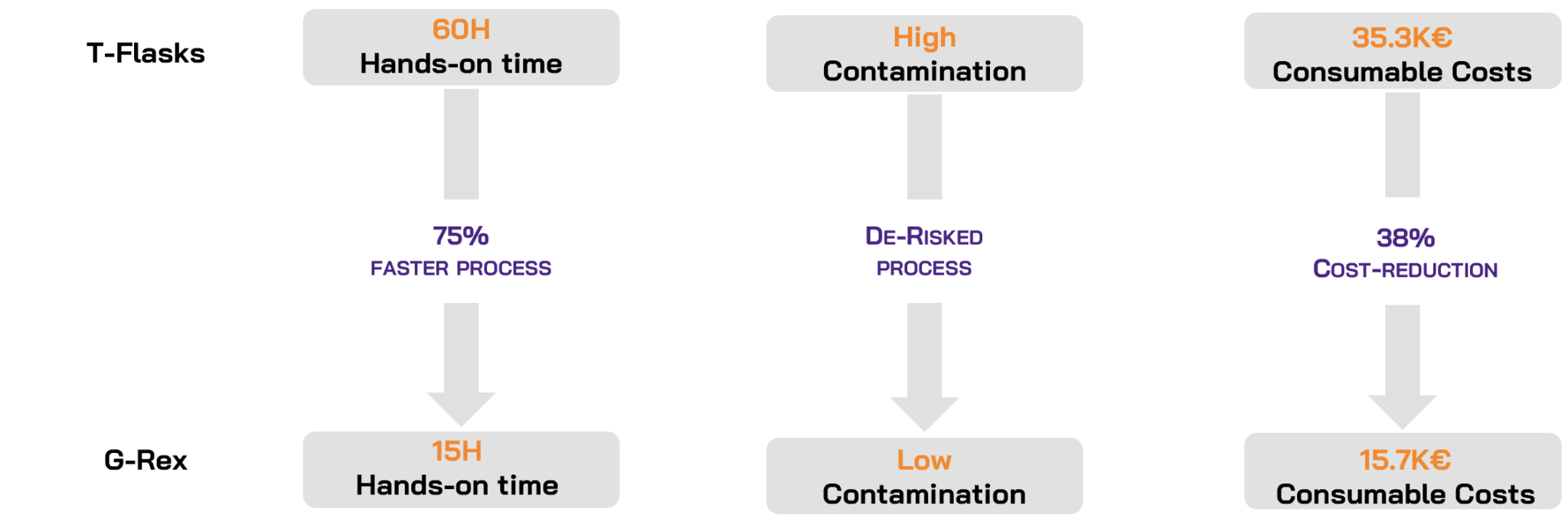
Challenge: You know how T-Flasks are the go-to in the lab? They’re simple, familiar, and they work perfectly at a small scale. But as soon as you try to scale up, you hit a wall. They consume a lot of materials, require tons of manual work, and contamination risks go up. For large-scale cell therapy production, they just can’t keep up.
Our solution: We replaced a 100‑T‑flask culture system with two G-Rex bioreactors. This setup allows dense cell growth with far fewer devices. Handling and equipment needs dropped, labor costs went down, contamination risks shrank, and cell quality stayed high.
2. Enhancing T-flask Process Robustness, Reducing Contamination Risks
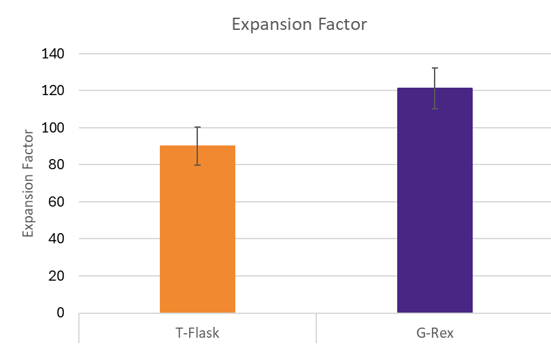
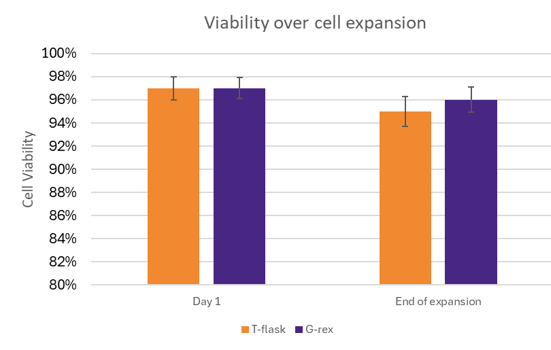
Challenge: T-cells are very sensitive to their environment. The main challenge was to scale up their expansion while ensuring high-quality cells, at least matching the results achieved with T-flasks.
Our solution: We approached it by carefully optimizing seeding density and culture conditions and validating the process across multiple donors. The result? Consistent expansion that actually exceeded T-Flask performance, achieving over 100-fold growth. Cell viability remained high at ~96%, on par with standard T-Flask cultures.
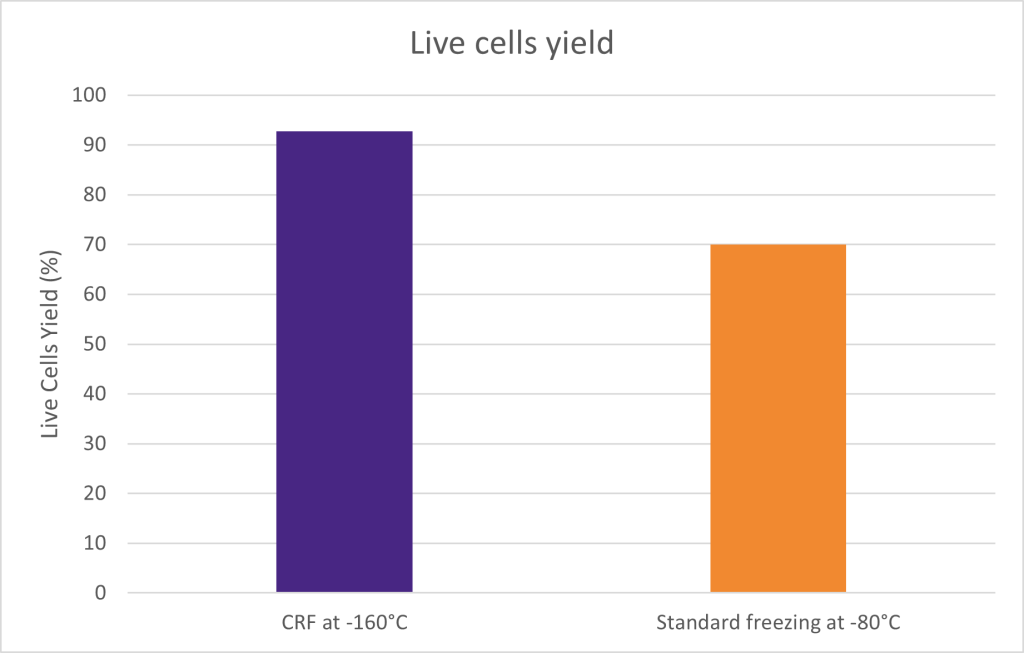
3. Increasing Cell Viability and Yield through Controlled Freezing Strategy
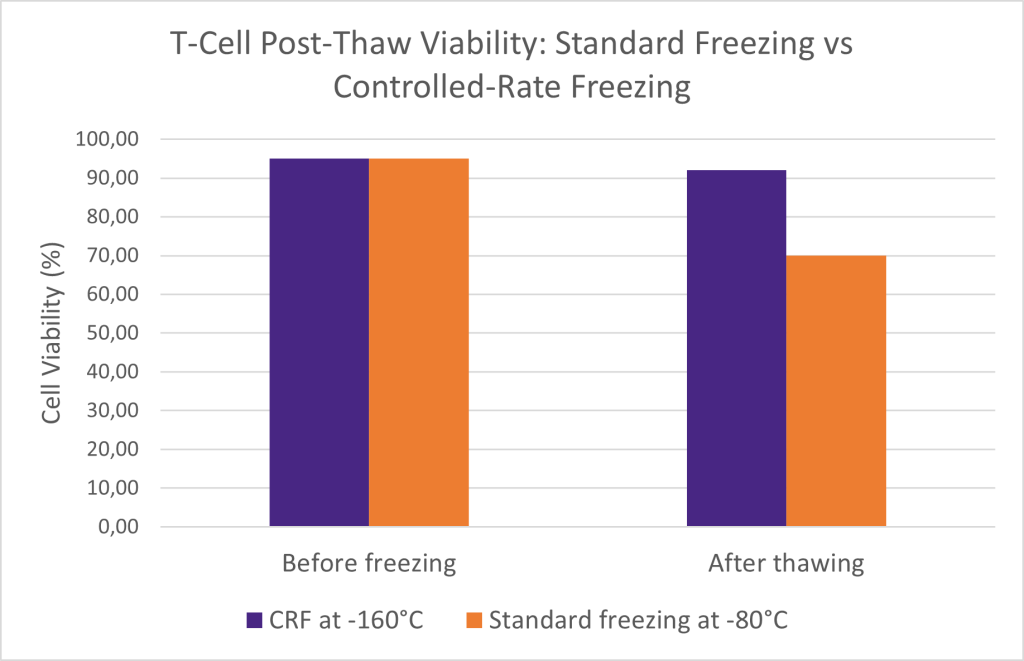
Challenge: Freezing and thawing T cells is a critical step that can significantly affect viability, membrane integrity, and recovery efficiency. Poor cryopreservation can compromise downstream experiments and in vivo studies, which are costly and highly dependent on high-quality cells.
Our solution: To address this, we developed a controlled-rate freezing protocol, carefully lowering the temperature at a precise rate of -1°C per minute down to -160°C to minimize cryo-injury. We systematically evaluated different cell concentrations to identify the optimal freezing conditions. The outcome was remarkable: post-thaw viability consistently reached up to 92% across donors and conditions and with a 93% yield of live cells, all while maintaining the T-cells’ immunophenotype. In other words, key surface markers remained intact, and the cells returned healthy and that predict full functionality.
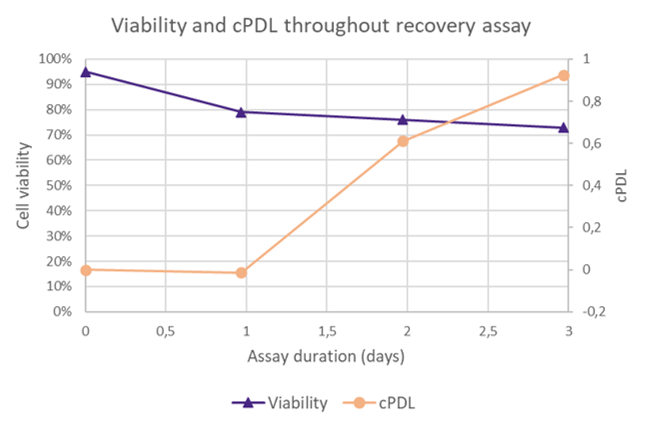
4. Controlling medium-term T cell performance
Challenge: Assessing T-cell viability and quality immediately after thawing often provides only a partial view of their true biological state. Even under optimized cryopreservation conditions, T cells can display delayed stress responses, progressive apoptosis, or gradual loss of quality over time. This can have a direct impact on both in vitro and in vivo studies, where cell recovery and sustained activity are essential for meaningful results.
Our solution: To capture these temporal effects and better predict downstream performance, we developed a medium-term recovery assay designed to monitor viability and cumulative population doubling level (cPDL) over several days. As anticipated, we observed an initial drop in viability immediately after thawing, which then stabilized at approximately 70% over the following days. The cells recovered their full growth potential within one to three days, demonstrating that the recovery process was consistently reliable.
Results and outcome
Conclusion
For biotech companies entering or approaching preclinical trials, it’s important to recognize that a “lab-scale process” is not the same as a “pharma-ready process”. We frequently see about one-third of cell therapy programs encounter significant delays simply because the original plan did not account for scalability. This often leads to costly and complex adjustments late in development.
The strategic solution is to consider scalability from the outset. You don’t have to navigate this alone: if you’re uncertain whether your process is truly scalable, or are already facing challenges with in vivo studies, a conversation can be invaluable. We can help you address these challenges and identify the most efficient path forward for your program.